Vaginosis – Distinguishing between BV, LV and CV
As if our vaginas were not already complicated enough, an imbalance of bacteria can turn them into a faucet for abnormal discharge. Common accompanying symptoms can include burning, itching, fishy odor, and painful sex. Untreated vaginosis can make you miserable during the day and keep you awake at night, not to mention ruin your sex life.
There are three sub-types of vaginosis: Bacterial, Lactobacillosis and Cytolytic. All result from an imbalance of healthy vaginal flora. All have symptoms that overlap with one another, as well as share symptoms with a candidiasis infection.
Depending on the type of vaginosis, signs, symptoms, and treatment options will vary. Knowing which type of vaginosis you have is crucial to proper treatment and should be diagnosed by a physician.
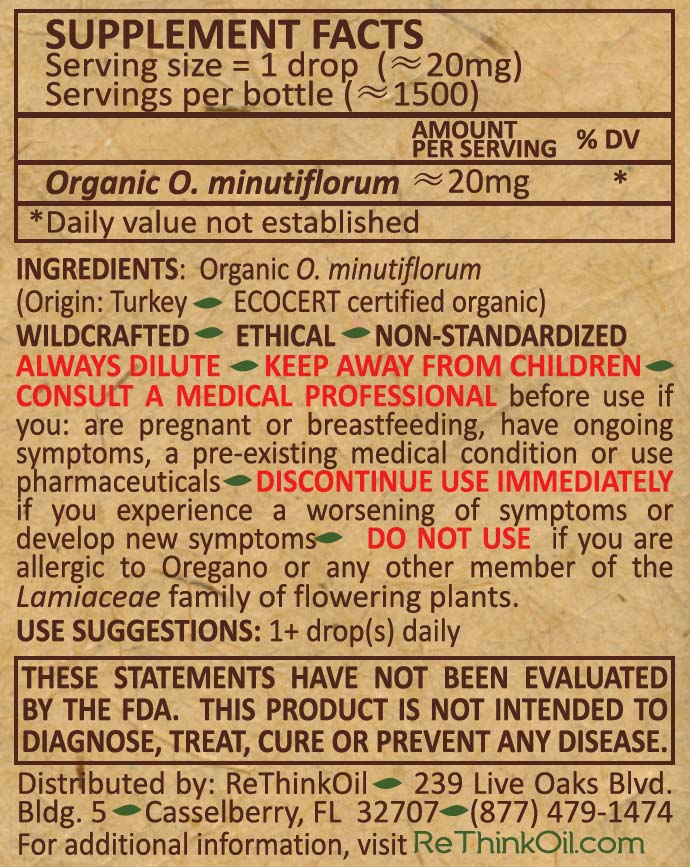
Oregano is a well-studied natural antimicrobial that can be utilized to rid the body of excess bacterial and fungal overgrowth.
Suggestions for using Oregano for BV symptoms:
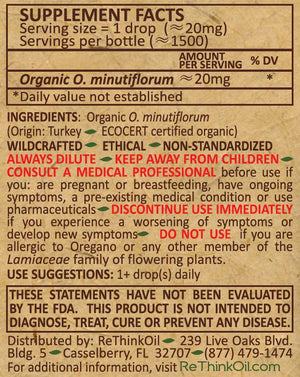
ReThink's Pure Oregano Essential Oil
Symptom management - properly dilute 3-5 drops of oil into carrier oil of choice, take 3x daily for 4-5 days.
Preventative - properly dilute 3-5 drops of oil into carrier oil of choice, take once daily or every other day.
ReThink's Oil of Oregano (1:4 dilution)- each 5 drops of oil of oregano = 1 drop oregano essential oil
Symptom management - Take 15-25 drops 3x daily for 4-5 days.
Preventative - Take 15-25 drops once daily or every other day.
ReThink's Oregano Capsules (WildCaps)- each capsule contains 5 drops of oregano essential oil (100 mg).
Symptom management - Take 1 capsule 3x daily for 4-5 days.
Preventative - Take 1 capsule once daily or every other day.
Whether you choose to try natural methods or traditional prescription therapy, proper genital hygiene should be practiced.
PROPER GENITAL HYGIENE
1. Wiping from front to back.
2. Washing with warm water only.
3. Avoiding scented soaps and feminine hygiene products.
4. Avoiding douching, tampons, steroid creams (unless prescribed).
5. Wearing cotton underwear.
6. Avoiding constricting, tight fitting clothing.
7. Performing monthly vulvar self-examinations (WARNING GRAPHIC CONTENT!).
8. Sleeping without underwear.
Those who are self-treating with natural antimicrobials (antibiotic, antibacterial and antifungals) should monitor symptoms closely during treatment and contact a medical professional if warranted.
COMPARISON CHART - CANDIDIASIS, BV, LV and CV


References: 1,2,3,4,5,6
1) http://ispub.com/IJANP/6/1/12743#
2) https://www.sciencedirect.com/science/article/abs/pii/S000293781290736X
3) https://www.cdc.gov/std/bv/stdfact-bacterial-vaginosis.htm
4) https://www.mayoclinic.org/diseases-conditions/bacterial-vaginosis/symptoms-causes/syc-20352279
5) https://www.womenshealth.gov/a-z-topics/bacterial-vaginosis
6) https://www.jcgo.org/index.php/jcgo/article/view/294/121