What causes the otherwise harmless candida yeast to proliferate into infections invading the skin, mouth, throat, esophagus and vagina- not to mention invasive infections that infect the blood, heart, brain, eyes, bones and elsewhere? (1)
The answer to this question oftentimes lies within the gut, where our immune responses are highly regulated. Chronic inflammation in the gut disrupts the balance of flora, allowing otherwise harmless candida to proliferate into candidiasis. If we have enough, our good bacteria will keep the bad bacteria in check so that it remains harmless.
There are various contributing factors that can disrupt the balance of flora, setting the stage for otherwise harmless fungi and bacteria to run rampant.
Contributing Factors
These factors include, but are not limited to the use of: Antibiotics, Steroids and Nonsteroidal Anti-Inflammatory Medications (NSAIDs). The Standard American Diet (SAD)- high in sugar, fat, additives and preservatives (mostly in the form of processed and fast foods) also contributes to the imbalance of gut bacteria.
Recognizing these common factors will afford you the opportunity to maximize your treatment protocol, with the goal of breaking the candida proliferation cycle.
Preventative/Treatment Measures
Diet is the first line of defense against candidiasis. Refined sugars and refined carbohydrates that turn into sugars provide candida access to an all-you-can-eat buffet, allowing for rampant proliferation.Failure to remove sugars will only prolong the treatment protocol.
For the best outcome, a diet free from refined carbohydrates and refined sugars should be followed throughout the treatment protocol. Doing this will allow antimicrobials to do their job more efficiently, without the continual proliferation cycle in play.
Those who are unwilling or unable to follow a diet free from refined sugars should consider adding in digestive enzymes with each meal or snack to assist in the break-down of ingested sugars, minimizing candida proliferation.
Antifungals are designed tokill fungal overgrowth, however there are known issues with effectiveness and reoccurring infections (due to antifungal drug resistance).
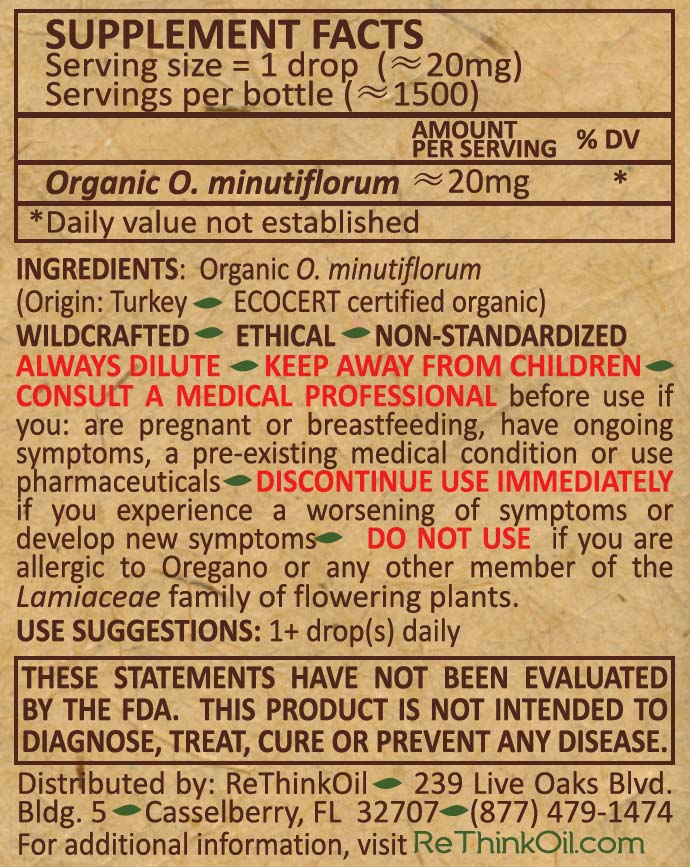
Natural antifungals can be used to enhance the effects of prescription antifungals, and even work to "reverse resistance".
"The selectively fungicidal characteristics and ability to restore fluconazole susceptibility in resistant isolates signify a promising candidature of thymol and carvacrol as antifungal agents in combinational treatments for candidiasis."(2)
Some commonly used natural antifungals include oregano, olive leaf, black seed, pau d’arco, caprylic acid, undecylenic acid, garlic, berberine, echinacea, grape seed extract, aloe and biotin.
Probiotics replenish the good bacteria as the yeast is being killed off.Good bacteria in sufficient amounts is required to keep overgrowth at bay.
Beneficial probiotics used during candidiasis treatment include strains of Lactobacilli (rhamnosus, acidophilus, lactis, casei, paracasei, plantarum, reuteri and fermentum) and Bifidobacteria (bifidum, animalis and breve). Although not a probiotic, S. Boulardii is a transient yeast that is used as a probiotic to assist in repopulating friendly bacteria in those with candida.
The strains rhamnosus, caesi and bifidum are especially helpful to assist in the digestion of toxins that naturally shed as a result of cell death from both fungi and bacteria. These toxins are responsible for the die-off symptoms (herxheimer reaction) that some people experience when using natural antimicrobials.
Antibiofilm agents will work to degrade the biofilm that naturally forms to protect candida from treatment. This is a normal defense mechanism for fungi and bacteria and is oftentimes associated with the chronic infection cycle.
Chronic fungal infections oftentimes involve stubborn biofilms & persister cells.Breaking through the biofilm and persisters is required to expose the protected candida, allowing it to be killed off by antifungals. Read more about biofilm here.
Although many natural antimicrobials also have antibiofilm properties, tough infections may need extra antibiofilm treatment to expose the underlying fungus. Some natural antibiofilm agents include oregano, black seed, curcumin, berberine, boswellia, ginkgo, bromelain, papain, quercetin, trypsin, serratiopeptidase, ozone therapy, NAC, zinc, iron and EDTA.